
How To Use Cannabis To Manage Chronic Pain
Published on 3/10/22
"Pain" is more complex than we give it credit for. When Dame Cicely Saunders introduced the concept of "total pain," which includes physical, emotional, social, and spiritual distress, she helped foster a revolution in medical professionals' idea of what pain constitutes. They began to understand that there are many different kinds of pain, and they all often feed into one another. Physical and chronic pain is often worsened by issues that cause mental anguish like anxiety and depression. Even the idea that you might not get better or relief from the current pain you're in can make existing illness and suffering worse.
Total pain also asks us the all-important question:
"What is the actual source of pain, and what is the best way to treat it?"

That's why pain requires a variety of different treatment methods. Yes, it's important to treat the physical source of pain, but it is just as important to also treat the depression and anxiety that accompanies the everyday grind of dealing with chronic physical pain. Many people who suffer from chronic pain are prescribed a chemical cocktail of different drugs, depending upon the severity of their pain, including analgesics (e.g. tylenol), non-steroidal anti-inflammatory drugs (NSAIDs e.g. ibuprofen), beta blockers, steroids, benzodiazepines, antidepressants and ultra-addictive opioids, just to name a few.
Whilst some of these medications have their potential and practical uses, they all share the same massive downside: the biggest risk factor with all of these medications is the potential for overdose, and when taken together they compound one another and make that potential overdose even more likely.
For example, even everyday analgesics like tylenol can increase the strength of opioids, raising the risk of overdosing and becoming dependent. Moreover, flooding your system with pill after pill will take a physical toll on both your physical and mental health.
Opioids are generally effective at beating physical pain, but they are dangerously addictive and come with a whole host of other unpleasant physical side-effects like dizziness, nausea, vomiting and constipation, just to name a few. Benzodiazepines are also often prescribed along with opioids for chronic pain, despite a lack of evidence for their efficacy for it and the potential for negative reactions with opioids.
This asks another important question:
"Are we effectively treating pain if we're just replacing one type of pain with another?"
That's where cannabis comes in. When it comes to safe, effective and more natural forms of dealing with pain, it's hard to beat the physical and mental effects cannabis can have on someone. There's a reason cannabis has been used as medicine for thousands of years, after all.
Table of Contents
- Cannabis As A Medicine For Pain
- Using Medical Marijuana To Treat Headaches and Migraine Pain
- Is there a cannabinoid-terpenoid profile and method of ingestion that is "best" for headaches and migraines?
- Using Medical Marijuana To Treat Back & Neuropathic Pain
- Using Cannabis to Treat Muscle Pain
- How To Replace Your Opiate Medication With Cannabis
- Cannabis Strains That Can Help Replace Opiates & Opioids
- Cannabis, Pain and Insomnia - What's the Relationship?
- Find Out More
Cannabis As A Medicine For Pain
The potential for the future of cannabis-derived medicine is virtually bottomless. While cannabis has been used as medicine for thousands of years before now, modern science helps understand exactly how and why cannabis-derived medicine works on your brain, nerves and cannabinoid system to effectively treat a long list of health issues.
For example, due to the entourage effect and the variety of naturally-occurring cannabinoid compounds available in the cannabis plant, many different types of pain can be treated in one simple and safe medicine. Why would patients take a whole host of pills, all designed for different purposes, all telling your body to do different things and often prescribed to treat the issues caused by the other medications themselves, when you can use one cannabis-derived medication that covers them all? This is just one very good reason why cannabis seems so popular for chronic pain amongst patients with all sorts of conditions.
Here are a few examples of the types of pain cannabis and cannabinoids may help patients manage.
Using Medical Marijuana To Treat Headaches and Migraine Pain
Headaches and migraine are complex conditions, perhaps mostly due to the fact that no one really knows where they come from. That lack of understanding of exactly what causes migraines can be frustrating for those suffering with them, often subjecting the patient to experimental prescription treatments that might not even work in the first place. That process of trial and error when it comes to treatment can be long, tedious and, most importantly, end up not actually relieving the crushing pain that comes with a migraine.
There are thought to be a variety of potential causes for migraines and headaches, including:
- Inflammation
- Irritation of blood vessels
- Head injuries
- Infection
- Tumors
- Stress
- Allergic reactions
- Dehydration
- An increase in intracranial pressure
- Sleep deprivation
- Gastrointestinal disorders
- An underlying neurological condition
- Overuse of medication
- Sensitivity to external stimuli
Due to the huge number of conditions that can cause headaches, treatment varies widely. Often, headaches are separated into "primary" (not dangerous, but can be benign, including migraine) and "secondary" (potentially dangerous, and may be caused by a life-threatening or debilitating condition). Whether there is a common cause of all types of headache is not known, but one theory is that headaches could be caused by lack of serotonin.
A 2019 study in the Journal of Pain directly linked the use of cannabis with a 50 percent reduction of headache or migraine pain, with concentrates shown to be even more effective than just smoking cannabis flower. Another 2019 retrospective study found that an astonishing 88.3 percent of 279 patient sample reported improvement in their headaches after using cannabis, with more than half experiencing less headache frequency and nearly 40 percent reporting improved, more restful sleep.
Obviously, as we mentioned before, treating migraines and headaches can be a tricky business. But there are clear links between cannabis and at least some patients getting some kind of lessening in symptom severity and frequency.
Cannabis has also been shown to have some clear neurobiological mechanisms that can directly benefit those suffering from headaches and migraines, like:
Vasodilatory effects of THC, allowing more oxygen to get into the brain. THC also lowers blood pressure. Alpha-pinene, a terpene found in cannabis, also has bronchodilatory properties.
- Vasodilatory effects of THC, allowing more oxygen to get into the brain. THC also lowers blood pressure. Alpha-pinene, a terpene found in cannabis, also has bronchodilatory properties.
- Downregulation of cytokine production and inflammation by both THC and CBD.
- Increasing serotonin production via attenuation of the serotonin receptors.
- Some people have reported an increase in headaches after cannabis use, and some people also report "rebound headaches" after cessation of cannabis use. Smoking may also induce headaches in some, and there have also been reports that edibles are less effective. Headaches/migraines may be best treated with a mixture of both CBD and THC.
Is there a cannabinoid-terpenoid profile and method of ingestion that is "best" for headaches and migraines?
As with so many other health problems, the best treatment for headaches depends upon where the headache is arising from. Assuming no benzodiazepine-based medications are being used at the same time, starting with a tincture containing a high CBD ratio (e.g. 20:1) may be helpful, and then work down from there (e.g. 18:1, 9:1, 3:1, 1:1) to see which works best for you.

Another factor to consider is the role of anandamide, one of the two cannabinoids that are naturally produced in the human brain. Studies have linked anandamide deficiency with migraines and increased anxiety, and consuming cannabis is a fantastic way of relieving the painful effects.
Vaporizing may help for immediate effects when sudden headaches appear, but be careful of substances such as glycol in the extract you are using. Vaping cannabis will get the medicine into your system quicker than via tincture, so it's probably the go-to choice for rapid relief.
As for whether there are any specific strains that are useful for headaches and migraines, this is difficult to say. In our study, most patients preferred indicas, but this is not to say sativas and hybrids were not used as well. A 2019 study showed that which strain you actually do choose doesn't make a huge difference, however. Trying some indica strains high in CBD may be helpful, but this is not to say sativas and hybrids are not useful. Figuring out which strain of cannabis works best to treat your individual symptoms is highly personal. One strain that works great for someone else might do next to nothing for another person, and vice versa.
Despite all the unknowns that are still associated with migraines, headaches and the treatment of them, we know that cannabis can at the very least play a role.
How Do I Use Medical Marijuana for Back Pain or Neuropathic Pain?
When it comes to treating back and sciatica pain with natural cannabis-derived medicine, the profile of what to do is very similar to treating migraines. Some experts estimate that as many as 40 percent of people will experience some type of lower back, nerve pain in their lives. Many opt for treating that pain with prescription painkillers like opiods, but medical cannabis is an effective and less addictive option as well. You'll just need to figure out which dosage is right for you.
With dosage in mind, much of the advice given above regarding which cannabinoid-terpenoid profile and strains to use for headaches and migraines applies here to back pain, too. You should start off with a tincture high in CBD-to-THC ratio (e.g. 20:1, 18:1), and then if that does not work, try a tincture with a different ratio (e.g. 9:1, 3:1, 1:1), ideally working down in stages. You may also find that you prefer different ratios for different times of day.
See what works best for you personally, as different people respond differently to different issues.
Also, as pain of all types tends to affect sleep, terpenes such as myrcene and linalool and the THC itself may be more helpful in getting to bed than looking at CBD alone. We already mentioned the power of the entourage effect, which boosts the power of cannabinoids when they're used together. Indeed, high CBD may keep some people awake! Beta-caryophyllene also has many painkilling properties.
Yet, there are some different treatment methods when it comes to back pain. Topicals and transdermals could be of use to treat localized nerve pain associated with back pain, alongside tinctures. CBD may also enhance healing in fractures. When it comes to spinal injuries, as well as neuropathic pain (nerve pain), indicas were overwhelmingly preferred by patients in our study. CBD was also much sought-after. THC, which mimics anandamide, will likely also control inflammation.
CBD, meanwhile, binds to TRPV1, which controls pain perception, as well as raising endocannabinoid levels in the brain's synapses. CBD, despite having little affinity for CB1 and CB2 receptors, seems to control the levels of cannabinoids available overall. To what extent this is so, it is not known, but it certainly gives CBD a very unique pharmacology.
Acidic cannabinoids, as well as THC, CBD and beta-caryophyllene, could be of huge use for back pain. Linalool, myrcene, humulene, limonene, alpha-pinene and beta-pinene are terpenes that may be useful for their painkilling properties. A mixture of cannabinoids and terpenoids may be best for neuropathic pain.
How Do I Use Medical Cannabis to Treat Muscle Pain?
Many of those suffering from neurological conditions are likely to suffer from muscle pain as well, due to all the cramps and spasms that are often associated with such conditions.
Athletes and those who are generally active are also likely to be prone to muscle pain and injuries, so having a natural, non-addictive way of relaxing the muscles and easing aches and pain safely without the use of harsh pharmaceuticals is important. Terpenoids such as linalool, which is found in jasmine and is often used in massage and bath oils, can help aid relaxation. There is some suggestion that CBD may reduce the amount of spasticity a person feels, and there is much evidence that CBD does seem to act as both an anticonvulsant and antispasmodic. THC, too, seems to help prevent spasms and therefore cramping.
How Do I Replace Opiate- or Opioid- Based Medications With Cannabis?
As cannabis can have negative interactions with many kinds of opiates and opioids, decreasing the amount of opiate-based medications taken over the course of the day will be necessary. Sadly, for many, this also means withdrawal symptoms arising from opiate addiction.
Fortunately, cannabis can provide a crutch to some extent, beating cravings whilst also working to ease the pain you're experiencing.THC and THCA could be of use for withdrawal, but other cannabinoids and terpenoids also help due to their painkilling and anti-addictive properties as well.
CBD and THC are could also be an "exit" away from opioids, as cannabinoids can be used to affect opioid receptors without the need to use opiates. Cannabinoid receptors seem to "cross link" and "talk" to one another, so cannabis may somehow tell the opioid receptors to "quiet down!"
Preliminary studies have even shown that patients using medical cannabis just took less opioids overall, which means two things. First, it shows that cannabis is comparable, if not even better than opiods, at treating people's pain. Second, it means that patients dealing with chronic pain can slowly reduce their dosage of opioids while increasing their dosage of cannabis without dealing with the pain and withdrawal symptoms that come with decreasing dosage.Due to their synergistic reaction, slowly tapering off of opioids and using small doses of high-THC cannabis may be necessary.
Other treatment methods may also need to be utilized, such as lifestyle changes, counselling and naloxone, but any treatment method that avoids the use of other opioids and benzodiazepines may be ideal in order to truly beat opiate addiction. Cannabis is a far safer, more natural bridge away from drugs currently administered for the treatment of opioid misuse.
Cannabis Strains That Can Help Replace Opiates & Opioids
Whether there's any particular strain or cannabinoid-terpenoid profile that is particularly useful for opioid addiction is, once again, difficult to say. High amounts of THC may help in the initial stages of opioid withdrawal, and then slowly lowering the amount of THC as cravings subside. Beta-caryophyllene, myrcene and humulene may also help. Edibles, tinctures and concentrates maybe ideal for opioid withdrawal.
Strains such as Gorilla Glue, White Rhino/Medicine Man, Super Silver Haze and Strawberry Cough may be useful, but the name alone does not necessarily tell you which strain has a high concentration of THC and other cannabinoids and terpenes - only testing can do this.
Is There a "Best" Weed for Headaches and Different Kinds of Pain?
Not necessarily, as what works well for one person may work differently for someone else. However, there are patterns of sorts that doctors and patients have noticed over time.
For inflammation, neuropathic pain and headaches, CBD and beta-caryophyllene may be quite effective. For chronic pain where opioids may otherwise be prescribed, as well as pain associated with treatments like chemotherapy, some more THC may be appropriate to help distract from the pain. THC also increases the appetite, which can be helpful if a patient isn't eating properly. Other cannabinoids and terpenes also contribute to cannabis' anti-inflammatory and pain killing properties, so isolates may not be as useful as more balanced cannabinoid-terpene profiles.
Cannabis, Pain and Insomnia - What's the Relationship?
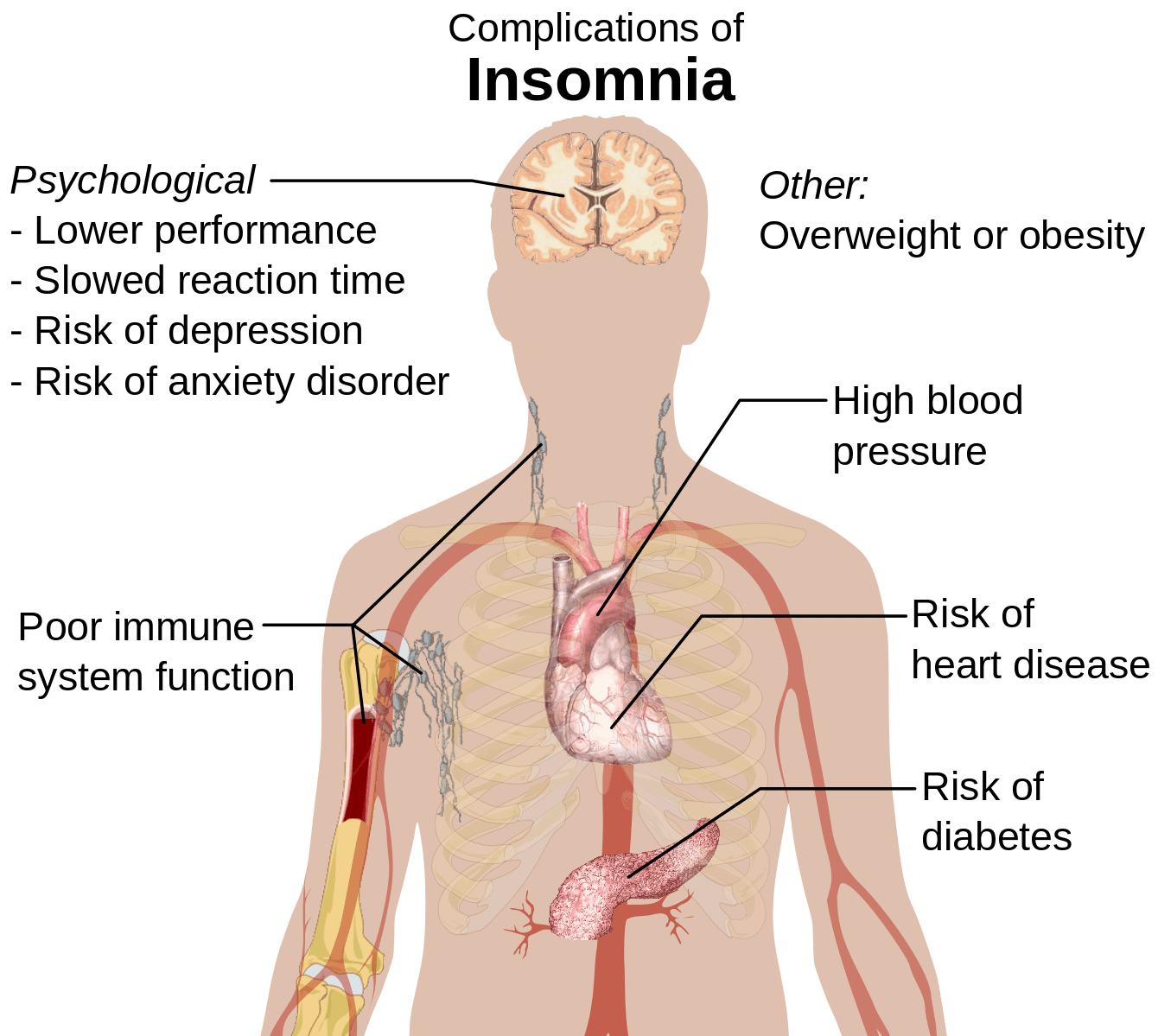
There is a link between pain and insomnia, and most chronic pain patient report having sleep troubles. Moreover, a lack of sleep can increase the likelihood of infection and the chances of getting ill, cause inflammation, cause headaches & migraine, and increase joint & nerve pain. Fibromyalgia and migraine sufferers may develop musculoskeletal pain due to long-term insomnia.
Nobody knows precisely what the link is between pain and insomnia. However, as pain detection, the sleep cycle and the immune system & inflammatory processes (as well as anxiety and depression) are all interlinked, it is reasonable to believe that the endocannabinoid system (ECS) is involved. While nobody knows the exact reasons why, it makes sense on the surface. If you're constantly aware of pain, it's harder for your body to relax and sleep. Over time, that lack of sleep when the body repairs itself leads to the worsening of the issues that keep you awake in the first place. It's a horrible cycle that just a little bit of CBD-rich cannabis can help ease.
Find Out More
If you'd like to know more about cannabis and its painkilling properties, check out our page on chronic pain. In more than a few instances, replacing prescription painkillers with cannabis has made a hugely positive impact on people's lives. When it comes to beating pain, there are few medications that compare with cannabis' ability to treat all aspects of total pain, whilst at the same time being generally quite safe. It is no wonder that chronic pain is one of the most common uses for medical cannabis.
